Market Intel: Nanorobots, Digital Tracking, Dose Printing: Innovative Drug Delivery Systems Will Make Precise Drug Dosing A Reality
Executive Summary
Precision medicine delivered by novel drug delivery systems, ranging from sensors to dose printers, could eventually revolutionize the pharmaceutical industry. Although many of these technologies are years away from commercialization, their ability to provide exact dosing with slow sustained release and more targeted therapy should improve patient compliance and outcomes.
Precision drug-delivery devices with the ability to provide precise doses of drugs to specific sites or tightly-controlled sustained release of a drug are poised to transform many sectors of medicine.
Digital Tracking System
On Nov. 13, 2017, the FDA approved the first drug in the US with a digital ingestion tracking system. Abilify MyCite is a pill with a sensor that digitally tracks if patients have ingested their medication and is approved for treating schizophrenia, bipolar disorder and depression. (Also see "First ‘Digital Medicine’ Approved, Slow Rollout Planned" - Medtech Insight, 15 Nov, 2017.)
Redwood City, California-based Proteus Digital Health Inc. developed the wearable sensor and Otsuka Pharmaceutical Co, Ltd. will market the drug.
“At Proteus, we have created a set of technologies that enables silicone and software to be integrated into a pharmaceutical product,” Andrew Thompson, Proteus' cofounder, president and CEO told Medtech Insight. “The first step was for these technologies to be approved as devices and then create a pathway, so they could be approved as combination products, whereby the drug and devices are working together.”
The first biotech drug, Eli Lilly & Co./Genentech Inc.'s insulin Humulin for diabetes, was FDA-approved in 1982, and now 35 years later. Fast-forward to today, where digital medicine “includes a drug that is formulated with an ingestible sensor, so that when the drug is swallowed, it is turned on to communicate,” Thompson said. “Once the drug is communicating, there also needs to be a device on the patient that detects the medicine and measures physiology.”
The wearable sensor, an adhesive patch that's worn on the abdomen, records vital information such as the time when the patient took the pill. It also measures daily activity levels and heart rate.
Figure 1 Proteus Digital Medicine Proteus Digital Health
“That information is then Bluetooth-communicated into a software architecture, first on an app on the patient’s mobile device, and then to the care team and family members invited by the patient,” Thompson said.
Proteus' goal is to improve outcomes associated with managing chronic conditions. “Currently, the medication possession ratio is around 50% and within that, you have some level of appropriate use of drug that is well below 50%,” Thompson said.
Physicians often rely solely on asking patients questions when deciding whether or not to change prescriptions. “But with digital medicines, we can provide physicians with completely objective and very precise data about how patients use their medicines and how they respond to them,” Thompson said. “As a result, doctors are much more able to engage with patients, who can make better health decisions about use of drugs and modify their lifestyle.”
It would also allow physicians to make better decisions about titrating, rotating or eliminating a drug. “People who use digital medicines take them between 85% and 95% of the time, which is a significant increase over normal rates,” Thompson said.
Company studies comprising patients with cardiovascular disease and metabolic conditions such as hypertension, diabetes and hypercholesterolemia have shown better outcomes, he added. Proteus is also developing digital medicine for infectious disease such as hepatitis C; and currently has three ongoing National Institutes of Health-funded studies using Proteus Discover in high-risk HIV patients.
In addition, the sensors are also being explored for applications in oncology, among others, Thompson said.
Dose-Printing
Dose-printing, vapor-jet printers embedding multiple medications onto a single surface, is another promising drug delivery system currently investigated by researchers is. (Also see "Market Intel: How 3D Printing Can Enhance And Expand Medtech Opportunities" - Medtech Insight, 7 Sep, 2017.)
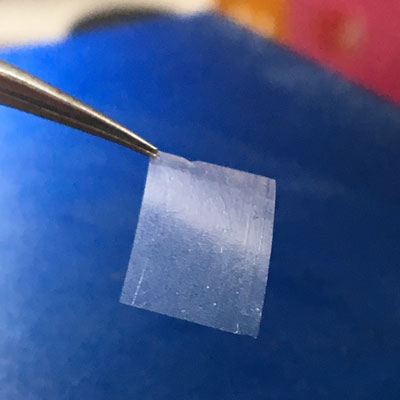
Figure 2

Microscopic image of nano- and- microstructured active pharmaceutical ingredient film printed in the Shtein Lab
Olga Shalev
“I am excited that dose printing provides unprecedented control over dosage, dose combining and scalability,” Max Shtein, a professor of materials science and engineering at the University of Michigan in Ann Arbor told Medtech Insight. Shtein's laboratory has created dose-printed small molecular pharmaceutical compounds for years. “Dose printing is also a natural extension to increasingly data-driven and data system-coupled medicine," he said.
With dose printing, the active ingredient of a drug can be heated to begin evaporation. “Pure nitrogen gas can then be used to pick up the vapor and print it onto any surface,” Shtein explained. “No solvent is used, so there is no need for any drying steps or worries about contamination or disrupting the surface you are printing on.”
This is a "fantastic technology" for medical conditions such as cancers requiring extremely high potency drugs in small, very precise doses that are poorly soluble, he said. The technology may also have applications for local/topical treatments.
"Chances are very good we could apply the active ingredient onto a patch to treat neuroblastomas, for example," Shtein said. He predicts that transitioning dose printing to in vivo animal studies could begin as early as 2018 and be introduced to the market by 2020.
“But for some severe/orphan disease cases, the process might be accelerated substantially,” he predicted. “We would love to partner with experts in drug discovery, formulation and testing in any area of medicine to help with the needs of specific existing and emerging process bottlenecks or clinical applications.”
Dose printing is unique, because it "enables a new approach for R&D of medicines, yet also allows for scalability from pilot fabrication (e.g. a contract for early-stage trials) to production for a wider market," he said. Shtein likens the approach to what happened in the semiconductor technology decades ago. “This is a natural next step for the pharmaceutical industry,” he said.
Researchers have traditionally thought of drug dosing as a one-size-fits-all, single-dose approach. He foresees that in the not-so-distant future we'll see data-driven prescriptions with dozens of active ingredients in fractional amounts that even doctors and patients themselves wouldn't be able to keep track off. This, in turn, will require a new manufacturing and delivery approach.
"Our vapor jet printing technology allows one to create sophisticated combinations just as easily as simple ones," he said. "It really is in step with the advent of precision medicine.” The biggest hurdle in adopting dose printing, he said, is simply getting the word out to researchers, practitioners and manufacturers that such a technology and capability exist.
"Luckily, we have received many requests for our nearby colleagues to print various small molecular compounds," he said.
LayerForm
LayerBio Inc.'s LayerForm is a proprietary controlled-release technology based on layer-by-layer fabrication. LayerBio's CEO Ken Mandell told Medtech Insight that it is a highly tunable technology capable of incorporating various classes of drugs, including small molecules, biologics and nucleic acids, with biodegradable and biocompatible polymer ingredients.
Mandell, who cofounded LayerBio in 2013 with Paula Hammond, a professor of engineering at the Massachusetts Institute of Technology, said that macromolecular drugs, such as proteins and nucleic acids, are readily incorporated in their layer-by-layer films, based on their charge and capacity to form hydrogen bonds.
"Depending on how the different drugs and polymers are combined, we can tune the release to suit different applications,” Mandell said. This could be in the form of a free-standing drug delivery film or as a coating on a conventional medical device like a stent or bandage. The Arlington, Massachusetts company's bottom-up coating process, applies a layer of a polymer followed by a drug, and then repeats the process to build-up enough layers for the required drug loading.
Figure 3
Color photograph of a LayerForm freestanding film for drug delivery
LayerBio
Together with Santa Cruz, California-based SomaGenics Inc., LayerBio developed coatings that contained a new class of drug -- synthetic short hairpin RNA (sshRNA) -- targeting the enzyme prolyl hydroxylase domain protein 2 (PHD2). The synthetic short hairpin RNA blocks PHD2, enabling expression of natural healing factors.
LayerBio is currently working with an undisclosed major pharmaceutical partner to develop a novel product for diabetic wound healing. Mandell said the coated drug showed significantly accelerated wound healing in a mouse model of diabetic chronic wounds. “The medication is coated on the surface of the dressing and released spontaneously when applied to the wound,” Mandell said.
The partners are also developing a product for Achilles tendon repair that involves a drug-release coating on a biodegradable sheath that is applied to the tendon during the surgical procedure. "Our technology enables targeted delivery of drug directly to the affected tissue, without systemic side effects or diffusion of drug to surrounding tissues,” Mandell said. “This represents a new paradigm for precision micro-dosing and targeted drug delivery.”
LayerForm's potential applications reach beyond wound care and tendon surgery.
Historically, eye diseases have been treated with eye drops. In recent years, however, companies have increasingly introduced injectable ophthalmology drugs. (Also see "Market Intel: Micro-Invasive Glaucoma Implants Mark Hottest Growth Spot In Eye Surgery Products Market" - Medtech Insight, 27 Nov, 2017.) And this is where Mandell foresees yet another opportunity for layer-based technologies.
“Injectable sustained-release formulations have the benefit of reducing the treatment burden and improving compliance for patients," he noted. "We see an enormous opportunity to improve ophthalmology outcomes via targeted micro-dosing inside the eye with injectable formulations.”
Mandell hopes to start clinical studies testing the technology for glaucoma in 2020, but acknowledged that commercialization will be years away.
Market Outlook
Garrett Vygantas, managing director of venture investments for OSF Ventures, a part of Peoria, Illinois-based OSF HealthCare Innovation said the pursuit to prove efficacy of therapeutics through improved delivery models is a hot area. (Also see "VC Deals Analysis: 2016 Bucks The Trend As Investment Dollars Dip" - Medtech Insight, 10 Jan, 2017.)
The global investment banking firm Torreya valued the global pharma sector in 2016 at $1.13 trillion, which is 30% higher than previous estimates, Vygantas said. Novel drug delivery systems will represent about $1.7bn by 2021, Vygantas told Medtech Insight.
“'The right dose for the right patient at the right time' is a precision medicine mantra that naturally lends itself to better outcomes, rather than relying on statistical goals that are not as precise,” Vygantas said. “This will continually create value for stakeholders, not just for the drug innovators, but also for the end-users, by reducing side-effects and improving efficacy and hopefully lower cost over time, because you will have an increased treatment effect that could be very substantial.”
In November 2017 the FDA approved Abilify MyCite, a version of Otsuka Pharmaceutical Co. Ltd. ’s atypical antipsychotic Abilify (aripiprazole) incorporating the Proteus sensor, which is ingested with the pill and sends a message to a wearable patch. Vygantas said Proteus/Abilify’s combined active pharmaceutical ingredient with digital technology is compliance-driven. "There are different intervention modalities on the device side that have already worked through some of those barrier issues and incorporating innovation into a product development plan," he said.
“Clearly, this ingestible formulation is one route of delivery,” he said. “Researchers are working on advancements in subdural delivery too. But I think the lowest-hanging fruit are those products that can be ingested and are timed-released, as is currently the case with some of the products to treat the central nervous system (CNS).”
He exemplified the Medici Drug Delivery System, a minipump for diabetes, developed by Boston-based Intarcia Therapeutics Inc. The minipump, which is the size of a matchstick, allows subcutaneous delivery of continuous and consistent flow of the medication exenatide – a glucagon-like peptide-1 receptor agonist, he said.
The FDA already accepted the company's new drug application, which puts the Medici Drug Delivery System on track for marketing approval. While minimally invasive drug delivery such as by ingestion or subcutaneously are key, Vygantas said that next-generation systems are already in the works.
“However, the next-generation delivery systems will be more sophisticated, like intravascular products that will somehow have a targeted response to the right tissue. We have already seen that with monoclonal antibodies targeting the correct cell, tissue or organ," he said.
Similarly, newer anticancer products often have a payload delivered to the tumor itself. “These are well-established, drug-targeting modalities,” Vygantas said.
Vygantas noted that as with all emerging technologies, these systems will face significant challenges from regulatory issues, proof of concept, value proposition to high cost and reimbursement. "Therefore, these companies continue to study and publish the results of their studies," he said. "As they demonstrate improvement over existing modalities, and if the delta is high enough, payers and stakeholders will pay attention."
He noted that "payers never want to pay for an experimental therapy until there is a high degree of confidence that it will decrease overall cost to the system, not increase cost.” Currently, there isn't enough evidence to confirm that these emerging technologies will decrease cost.
“Further, often the price of these new products is high in order to recoup the significant amount of investment that has been made,” Vygantas said, noting that “These are very risky investments.” While established companies have limited their R&D to a few large-market therapeutic areas like cardiovascular and metabolic diseases, med tech start-ups can target smaller areas of unmet medical need, such as gynecology and ophthalmology, that require less investment dollars, he noted (Also see "Market Intel: Eye On The Prize: Drug Delivery Advances To Fuel Ophthalmic Drug Market" - Medtech Insight, 22 Aug, 2017.).
Wandering Robots
Bradley Nelson, a professor of robotics and intelligent systems at the Eidgenössische Technische Hochschule in Zurich, Switzerland, has been researching novel drug dosing systems for the past decade.
Nelson told Medtech Insight he's most excited about systems that target specific locations in the body for drug delivery. His research focuses on how microrobots and nanorobots can be used to carry and release drugs through the body (Also see "Market Intel: Ever Decreasing Dimensions, Snakes And Origami: The Next-Gen Surgical Robots" - Medtech Insight, 28 Feb, 2017.).
The concept draws parallels to the 1960’s science fiction movie, Fantastic Voyage, in which a submarine crew shrinks to microscopic size and navigates the body of an injured scientist to perform delicate brain surgery.
Video 1
Bacteria-sized robots for precision drug delivery/Bradley Nelson
World Economic Forum
One of Nelson's microrobots delivers drugs for age-related macular degeneration. Among the biggest challenges in making the technology successful is using magnetic fields to move devices as well as fabrication.
"We are still learning the challenges of what kinds of fields to generate,” he said. But he expects that within the next 10 years, researchers will find a way to bring these devices into humans.
Drug in Blood
Another company, San Diego, California-based Abreos Biosciences Inc. meanwhile, is developing a blood test it hopes will win FDA approval for precision dosing of expensive and powerful biologic therapies. (Also see "Market Intel: From AI-Based IVDs To Precision Drug Dosing: Medtech Conference 2017 Gives Insight Into Tomorrow's Technologies" - Medtech Insight, 9 Oct, 2017.)
“Our core technology is to measure the amount of drug in blood through a simple blood test, then give that information to the physician, so they can consider adjusting the timing of dosing, the amount of dose, or switch to a different drug as they see fit,” Abreos' CEO and cofounder Bradley Messmer told Medtech Insight. “Our goal is better patient outcomes.”
Messmer said that these drugs are typically given in a “one-dose-fits-all” approach, which has many negative implications. “We know this is not right,” he said. “Some patients are given more drug than needed, which can lead to increased side effects, while others are not given enough of a drug to achieve an effect."
There is a health economic benefit for not over-treating patients on one side and wasted spending for patients who are undertreated without positive outcomes on the other.
In September 2017, Abreos received a Phase II NIH Small Business Innovation Research grant to fund the development of a point-of-care test for rituximab (Rituxan), a costly drug used to treat leukemia and several autoimmune conditions. The lateral flow assay-based system is similar to a pregnancy test, yet quantitative, so that a finger stick of blood from the patient can be used to understand the drug level in 10 to 15 minutes,” Messmer said.
He hopes for FDA approval in 2019, but wants to develop a test that would allow patients to monitor drug dosing at home just as diabetes patients can monitor their glucose levels at home.
He said Abreos’ technology targets most biologics spanning across several therapeutic areas: neurology; autoimmune disorders with infliximab and adalimumab; and oncology with powerful immunotherapies like pembrolizumab.
“Still, the ways that precision dosing can improve patient outcomes vary by indication,” he says. “In general, though, for many biologics, research has shown that severe side-effects are linked with high drug levels. Conversely, patients with low drug levels do not respond to therapy.” Early next year, Abreos expects to launch its first commercial laboratory developed test for therapeutic dose monitoring of natalizumab for multiple sclerosis.
“For this test, blood is drawn and run in our lab,” Messmer said. “We are initially focusing on natalizumab, because of its associated risk of progressive multifocal leukoencephalopathy (PML), a brain infection which is very deadly. Researchers have identified an increased risk of PML in patients excessively dosed with natalizumab. We believe that precision dosing can help mitigate this risk.”
Messmer is convinced that it won't be long before precise drug dosing becomes the new normal. "It will be unthinkable that these powerful and expensive medications were not precisely dosed," he said.
One of the biggest hurdles, he said, will be acceptance and adoption of the new technology by physicians. "We are developing clinical evidence to help educate physicians on the need and the utility of therapeutic dose monitoring. The value of delivering the right dose to the patient seems self-evident, but creating the right strategy for the entire ecosystem of payer, provider and potentially pharma is indeed a daunting challenge," he said.
Proteus' Thompson finds that the megatrend in human behavior is shifting from models based on buildings, people and products to models based on software, service and mobile platforms. “Having your drug being a digital object over the next decade will become ubiquitous,” Thompson predicted. “Any medical condition where appropriate dosing is tied to outcomes would be a very good use of digital medicine.”
Dose titration is particularly relevant to hypertension for controlling blood pressure, treating mental health and managing pain, he said. “Personalized medicine is getting the patient on the right drug in the right dose at the right time, and at the right place and the right price,” Thompson said. “These unique therapeutic solutions are a new way of thinking about what a pharmaceutical product can be. The drug is part of a solution that includes software, data and analytics and the ability of patients to engage with their own care by making use of the mobile device in their pocket.”
Thompson noted that for 100 years, beginning in 1898 with synthetic aspirin from Bayer, the pharmaceutical industry had been relying on chemistry. “It also has been an industry in which R&D activity has halved every nine years for the last five decades; in aggregate it now costs about $10bn per drug to bring to market,” he said.
However, clinical studies for new drugs can't prove if a patient took the drug, he said. “But with digital medicines, we absolutely know with certainty whether a person took the drug, when it was taken and how the body is responding," he said. "That is going to become a ubiquitous feature of how drugs are discovered, developed and commercialized. As a result, digital medicines will enable the pharmaceutical industry to have a much more sustainable innovation and business model.”
From the editors of Clinica